Health and Well-being Week
Well-being ecosystem creation
Japan Association for the 2025 World Exposition
The programme, together with the General Sponsors, explores: 'How can data utilization be leveraged to enhance the well-being of a more diverse and extensive population?'
Recorded video available
Discussion
- Others
| Transmission of simultaneous interpretation | Provided |
|---|---|
| Language of interpretation | Japanese and English |
-
Agenda2025
Organised Programme
-
Time and
Date of
the event -
-
2025.06.28[Sat]
13:30 ~ 15:30
(Venue Open 13:00)
-
- Venue
- Theme Weeks Studio
Programme details
*Subtitles: Choose “Subtitles/CC” in the “Settings” (gear
icon) at the bottom right of the YouTube video.
*Subtitles may not show with multiple languages or overlapping
audio.
Health and well-being are human needs and closely tied to the
strength and resilience of societies and economies. This is
universal. Global stakeholders across sectors - patient,
government, health system, clinical, payer/employer - express
common challenges about how to achieve, measure, and sustain
both health effectiveness and efficiency. This panel will
explore the stressors and incentives that are centering
well-being as a global focus in policy, payment and care
delivery. Discussion will focus on defining best metrics,
identifying trends in incentives for change, and
prioritization of data for decision-making at all levels. Key
experience and perspectives from employer, regulator, payer
and patient communities will be shared.
Reports
【Program Summary】
This program, "Well-being ecosystem creation," was
held on June 28, 2025, as Agenda2025
Organised Programme during Expo 2025 Osaka, Kansai, Japan,
"Health and Well-being Week." Experts from around
the world, corporations, academic institutions, and healthcare
insurers gathered to discuss the question: *"How can we
enhance the Well-being of diverse and broad populations
through the utilization of data?"*
In this session, participants shared a comprehensive
definition of Well-being that goes beyond the boundaries of
health and medical care, encompassing mental, social, and
economic aspects. Each participant presented their approach
from their respective positions to identify common challenges
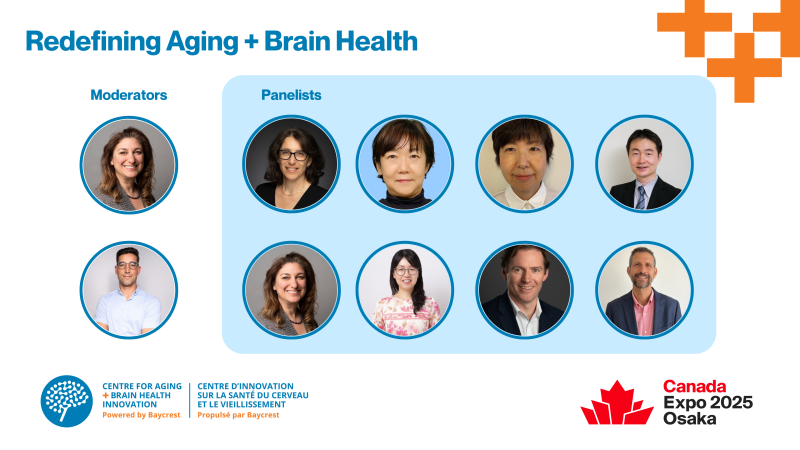
and visions. The moderator was Jennifer L. Bright from the
International Consortium for Health Outcomes Measurement
(ICHOM), and panelists included representatives from global
corporations and academia.
This program succeeded in presenting participants with
concrete frameworks and measures to evaluate and improve
Well-being, while also presenting a vision for a
"co-creation type healthcare ecosystem" that will be
required by society in the future. Furthermore, the importance
of continued dialogue and collaboration was strongly
emphasized, particularly regarding data quality and
utilization, as well as connecting the perspectives of
policymakers with those of practitioners and stakeholders on
the ground.
【Speaker Summary: Jennifer L. Bright】
At the opening of this session, Jennifer L. Bright presented a
systematic framework on the concept of Well-being and its
multidimensional measurement, providing a foundation for the
discussion. She first introduced existing Well-being
measurement indicators by international organizations such as
the OECD and WHO, emphasizing that they include complex
perspectives such as economic factors, health, education,
environment, governance, and life satisfaction. She also cited
the U.S. "Well-being in the Nation" framework,
stressing the importance of evaluations based on individuals’
subjective states, such as distress, struggle, and thriving.
Furthermore, she touched on the activities of ICHOM,
advocating for a global healthcare improvement framework
centered on evaluating quality of healthcare through
measurement of health health and life quality outcomes most
important to patients. She emphasized that health should not
simply be defined as the absence of illness but should be
composed of multifaceted elements such as mental health,
physical and social functioning, family relationships, and
employability. She underscored that the measurement of
Well-being is a common challenge for nations, corporations,
and healthcare providers. alike.
Bright questioned the tendency to regard Well-being as a
"soft topic," pointing out that with appropriate use
of data, favorable outcomes could be achieved without
increasing financial burdens. She raised the importance of
asking "why" when interpreting and using data,
stating that it is essential not to stop at the mere
collection of numbers but to interpret them with an
understanding of the background and cultural context and
reflect this in policies.
Finally, she emphasized that the promotion of Well-being is
not only an individual responsibility but a shared
responsibility of all stakeholders, including governments,
employers, healthcare providers, and insurers, stressing the
need for an all-inclusive approach that involves patients and
social participation to ensure relevance.
【Speaker Summary: Jeni Chih】
Jeni Chih, Senior Director of Global Benefits at PepsiCo,
shared how the company supports the health and Well-being of
approximately 400,000 employees in 72 countries worldwide.
Under the initiative named "Healthy Living," the
company has developed a comprehensive Well-being program built
around four pillars: physical health, mental health, financial
stability, and connection to the community, aiming to meet the
diverse needs of employees.
She particularly highlighted the importance of "care as
an experience," rooted in the company's philosophy
of care. Chih stated, "It is not enough to merely provide
benefits; employees must feel that they are valued." She
emphasized the need to consistently deliver physical, mental,
and social support to achieve this. In response to the issues
of loneliness, anxiety, and mental health challenges revealed
during the COVID-19 pandemic, the company has also actively
incorporated mental health support, communication initiatives,
and programs for employees’ families.
Chih also addressed the challenge of encouraging employees to
take action. She noted that even when health initiatives are
in place, whether individuals act on them ultimately depends
on their personal choice. She stressed, "The most
effective health manager is the individual themselves. No one
understands their own body and mind better than they do."
Through the message that each employee is "their own
superhero," she advocated the importance of self-directed
health behaviors.
She also discussed efforts to provide information to
non-employee dependents such as family members and spouses, as
well as navigation support using technology (e.g., the
"Fairy Godmother Project"), designed to deliver the
right information at the right time. Her talk left a strong
impression that corporate-provided Well-being should be based
on "relationships" and "trust," rather
than merely consisting of systems and initiatives.
【Speaker Summary: Dr. Margaret Kruk】
Dr. Margaret Kruk, who has worked for over 20 years as a
global health researcher focusing on healthcare system reforms
in low- and middle-income countries, presented the
achievements of global health improvements to date and the
challenges that remain. She first introduced the dramatic
reduction in mortality achieved globally in fields such as
HIV/AIDS, malaria, and maternal and child health, praising the
progress made in medicine through technology and
collaboration. However, she stressed that addressing the
remaining health disparities is essential.
She particularly focused on the question, "What is the
fundamental purpose of health systems?" Kruk proposed
that a high-quality healthcare system should be based on three
pillars: (1) consistently improving care, (2) earning the
trust and value of the population, and (3) flexibly responding
to the changing needs of the population. She argued that
rather than simply expanding access, it is necessary to focus
on the "quality" of the medical care provided and
called for the use of indicators directly linked to actual
health outcomes, such as control rates of chronic diseases
(e.g., hypertension).
Kruk stated that improving healthcare quality requires reforms
at the "structural level," including system design,
personnel placement, and incentive structures, rather than
just interventions at the field level. She introduced an
example from the United States on improving responses to heart
attacks, explaining that the success was only achieved through
comprehensive reforms of the entire system, from community
awareness to emergency systems, specialized treatment, and
rehabilitation.
She also presented findings from the "People’s Voice
Survey," a survey collecting feedback from citizens on
healthcare systems, revealing that in many countries, younger
generations and highly educated urban residents were more
dissatisfied with the system. This poses the risk of losing
the trust of the very groups who will become future taxpayers
and supporters of the system. She emphasized that gaining
citizens’ empathy and consent is essential for building a
sustainable system.
Concluding her talk, she quoted General MacArthur: "No
matter how beautiful the strategy, you should occasionally
look at the results," reiterating the importance of
operating healthcare systems based on outcomes. Her remarks
pointed toward the creation of a global healthcare ecosystem
that visualizes healthcare quality and builds it together with
citizens.
【Speaker Summary: Nils Reich】
Nils Reich, CEO of AXA’s Global Health Business, spoke from
the perspective of an insurer responsible for approximately
USD 25 billion in annual medical expenditures across more than
25 countries, discussing the challenges and possibilities of
realizing a sustainable healthcare ecosystem. He pointed out
that despite differences in healthcare systems worldwide,
common challenges have emerged, such as "medical cost
inflation" and "increasing difficulty of
access."
According to Reich, the rate of increase in medical costs has
been running 5–7 points above GDP growth rates, a structure
that is unsustainable in the long term. At the same time,
demand for insurance services is increasing, particularly with
strong needs from younger generations and corporate clients
for "secured access." He stated that insurers have a
responsibility not to simply pass on costs but to improve
healthcare efficiency and effectiveness.
Reich focused on the "power of data" as the
breakthrough, introducing specific examples of how his company
uses its data to assess healthcare quality and identify waste.
For example, he pointed out that the rate of morphine
administration after knee surgery varies greatly between
hospitals within the same country, suggesting that unnecessary
procedures might be performed contrary to patients’ best
interests. He explained that correcting such
"variations" is key to simultaneously improving
patients’ quality of life (QOL) and reducing costs.
He further stated that while digital technology and data
utilization for optimizing care will bring significant
transformations in the future, implementation requires
collaboration among diverse stakeholders and a shared vision.
"To achieve the greatest outcomes with the resources we
have, we must reduce unnecessary procedures and focus on
necessary care," he said, calling for the construction of
a "win-win-win" structure in which insurers,
healthcare providers, policymakers, and corporations act with
a common purpose.
Reich’s remarks strongly underscored that redefining the role
of insurers and adopting a data-driven approach will become
increasingly important for balancing economic rationality with
human-centered care.
【Speaker Summary: Daniel Erasmus】
Daniel Erasmus, speaking from the perspective of an actuary,
discussed the potential for visualizing healthcare outcomes
using data and designing patient-centered healthcare systems
based on that data. He emphasized that the perspectives of
various stakeholders in the healthcare ecosystem differ
greatly: insurers prioritize cost management, healthcare
institutions focus on technology adoption and maintaining
patient volume, regulators emphasize the sustainability of
systems, while patients care most about "improving their
own health." He advocated for healthcare that is centered
on patients.
Erasmus then cited the Australian healthcare system as an
example, highlighting that the cross-subsidy structure—where
support flows from younger to older populations—is collapsing
due to aging. He also noted that while the introduction of the
latest medical technologies has improved patient outcomes, the
costs and increased number of procedures have driven up total
healthcare spending. For example, with the introduction of
robotic surgery, high-risk patients who would previously not
have been surgical candidates are now included, resulting in
expanded demand for healthcare.
He also pointed out that "the health status at the time
of admission" has a significant impact on medical costs
and outcomes, stressing the need to pay more attention to
prevention and daily health management (social factors). He
explained that simply ensuring adequate nutrition before
surgery can significantly impact post-operative recovery,
underscoring the importance of improving patients’ conditions
before treatment as a perspective for making healthcare
systems more efficient.
Furthermore, Erasmus explained that his company, Insight
Actuaries, uses Patient-Reported Outcomes (PROs) data to show
that aspects of the "patient experience," such as
the quality of explanations and addressing anxiety at
hospitals, affect outcomes at six and twelve months
post-surgery. Even with the same medical procedures, if the
relationship with the patient is good, it positively impacts
recovery and self-management. Based on these findings, he
stated that they are working on developing
"understandable communication" using AI-based
language generation, which can adapt to patients from diverse
backgrounds, such as Indigenous people and the elderly.
Erasmus’s remarks compellingly indicated, from both data and
practical perspectives, that the key to maximizing healthcare
system outcomes lies in "co-creation centered on
patients," offering valuable insights for system
designers.
【Discussion Summary】
In the latter half of the session, moderator Jennifer Bright
asked each panelist multifaceted questions about the
possibilities and limitations of improving Well-being through
data utilization, as well as challenges in practice.
First, Chih spoke about the dilemma of companies having
abundant employee data but not being able to extract the
"cup of drinkable water (= meaningful data)" truly
needed. She stressed the importance of building trust with
partners and evaluating outcomes aligned with objectives. She
also highlighted the difficulty of delivering information to
non-employee dependents such as family members and spouses,
pointing out the necessity of individually optimized
navigation.
In response, Kruk stated that feedback from patients and
citizens is the key to improving systems, and the essence lies
in exploring "why good/bad results occur" rather
than simply conducting satisfaction surveys. She also touched
on the current situation where younger generations and urban
residents are dissatisfied with the system, emphasizing the
importance of securing trust from the next generation.
Reich asserted that by correcting "variations" and
"waste" in healthcare resources, it is possible to
achieve both cost containment and improved quality of life.
From a global perspective, he emphasized the significance of
insurers, corporations, providers, and governments working
together with a shared vision.
Erasmus stated that technological innovation is creating an
environment where the individual needs of patients can be
better understood, and to ensure that everyone benefits from
new technologies, it is necessary to balance the quality and
accessibility of outcome data. He also introduced initiatives
using AI to support communication that accommodates diverse
cultural and linguistic backgrounds, sharing his vision for a
"patient-centered co-creation ecosystem."
Throughout the discussion, a common understanding emerged that
the quality and meaning of data, as well as its interpretation
in context, should be prioritized over sheer quantity. The
session concluded that it is essential to focus on who the
data is for, what decisions it informs, and who will use it,
and that building a sustainable and inclusive Well-being
ecosystem requires a common understanding and collaboration
among multiple stakeholders.
Cast
Moderator

Jennifer L. Bright, MPA
President & CEO, International Consortium for Health Outcomes Measurement (ICHOM)
Jennifer Bright, MPA (she/her) is President & CEO,
International Consortium for Health Outcomes
Measurement (ICHOM), a nonprofit that works with
patients and clinical experts worldwide to define and
deploy standardized tools to measure health outcomes
that matter to patients. Prior, she held executive
roles at the Innovation and Value Initiative (IVI),
focusing on advancing patient-centricity, transparency
and equity in health technology assessment, at the
Society for Healthcare Epidemiology of America, and
Mental Health America.
Jennifer is also Founder and President, Momentum
Health Strategies®; Board Chair, Mental Health
America; and editor, American Journal of Accountable
Care and the Journal of Patient Experience. She holds
degrees in political science and public administration
from Trinity University and George Washington
University.
View Profile
Close
close
Speakers

Dr. Margaret Kruk
Distinguished Professor of Health Systems and Medicine, Washington University School of Medicine; Director of the QuEST Network
Dr. Kruk is Professor of Health Systems at the Harvard T.H. Chan School of Public Health. In January 2025, Prof. Margaret E. Kruk will become Distinguished Professor of Health Systems and Medicine in the School of Medicine at Washington University in St. Louis. Dr. Kruk studies how health systems perform in improving health and generating trust across countries. Working with colleagues in Africa, India, South America, and Europe, she develops novel measures of health system quality and measures how system performance affects population demand for health care, health outcomes, and confidence. Dr. Kruk and her team use implementation science and econometric methods to design and evaluate large-scale health system reforms. Dr. Kruk is Director of the QuEST Centers and Network, a multi-country research consortium working to produce a global evidence base for improving health systems. The QuEST Network responds to the findings of the Lancet Global Health Commission on High Quality Health Systems in the SDG Era (HQSS Commission), a global initiative chaired by Dr. Kruk. QuEST develops new instruments to assess health system quality, tests structural solutions to health system deficits, and supports expansion of high-impact health systems research in partner countries. Previously Dr. Kruk was Associate Professor of Health Policy and Management and Director of the Better Health Systems Initiative at Columbia University and Assistant Professor of Health Management and Policy at the University of Michigan. She has held posts at the United Nations Development Program and McKinsey and Company and practiced medicine in northern Ontario, Canada. She holds an MD degree from McMaster University and an MPH from Harvard University.
View Profile
Close
close

Nils Reich
CEO, AXA’s Global Health business
Nils Reich serves as the CEO of AXA’s Health and Employee Benefits business, operating in over 25 countries. Prior to this, he was responsible for AXA Group’s property and casualty insurance business in Germany and held several other executive positions and board memberships. Before joining AXA, Nils worked in strategy consulting, serving clients across four continents. He has been recognized as one of the ‘Top 40 under 40 in Germany’ and serves on the board of the Association of Arts and Culture of the German economy. He holds a PhD in Financial and Computational Mathematics from ETH Zurich.
View Profile
Close
close

Daniel Erasmus
CEO, Insight Actuaries
Daniël Erasmus is the CEO of Insight Actuaries with
nearly 20 years of experience in the healthcare
industry. His areas of expertise include developing
and designing value-based healthcare structures,
funding mechanisms, and service delivery models.
Daniël emphasizes the importance of prevention and
long-term market sustainability in his work.
He is also deeply interested in the future of
healthcare, particularly in how wearable technology
and patient-reported data can enhance wellness,
preventative care, and longevity. His expertise
includes optimizing value-based reimbursement
strategies to ensure better healthcare outcomes and
financial viability.
View Profile
Close
close

Jeni Chih
Sr Director, Global Benefits at PepsiCo
Jeni Chih is a seasoned leader with a proven track
record of driving innovation and transformation across
diverse industries. With a career spanning diverse
industries including manufacturing, investment
banking, retail and technology at renowned companies
such as Oracle, NetApp, and Gap Inc., Jeni has amassed
a wealth of experience in strategic design and
execution in global benefits.
Currently serving as the Senior Director of Health
& Wellness for design and strategy at PepsiCo,
Jeni leverages her diverse background to drive
impactful change at the intersection of employee
well-being and organizational strategy. In this role,
she leads initiatives to design and implement
comprehensive health and wellness programs that
prioritize the holistic needs of employees.
With her extensive experience, strategic mindset, and
commitment to making a positive impact, Jeni Chih
continues to drive meaningful change in the realm of
health and wellness, setting the standard for
excellence in design and strategy across industries.
View Profile
Close
close
Health and Well-being Week
Well-being ecosystem creation
The programme, together with the General Sponsors, explores: 'How can data utilization be leveraged to enhance the well-being of a more diverse and extensive population?'
-
2025.06.28[Sat]
13:30~15:30
(Venue Open 13:00)
- Theme Weeks Studio

OTHER PROGRAM
Health and Well-being Week